SUBINGUINAL MICROSCOPIC VARICOCOELECTOMYWe start with a 2–3-cm oblique skin incision centred over the external inguinal ring, as previously described. The incision is deepened through Camper's and Scarpa's fascias and the spermatic cord is then grasped with a Babcock clamp, delivered and placed over a large (1-inch) Penrose drain. The testicle is then delivered and the gubernacular veins and external spermatic perforators are isolated and divided (Fig. 1). The testicle is returned to the scrotum and the spermatic cord is elevated on a large Penrose drain. The microscope is then brought into the operating field and the cord examined under 8–15 power magnification. The internal and external spermatic fascias are incised and the cord structures are again examined (Fig. 2). 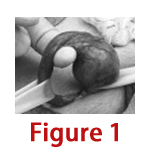 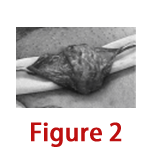
Testicle delivered through the subinguinal incision depicting the spermatic cord (held by Penrose drain; bottom left) and the gubernaculum (held by Penrose drain; right). Spermatic cord with Penrose drain beneth it (the internal and external spermatic fascias have been opened). To simplify the procedure and protect the vas deferens and its vessels from potential injury during subsequent cord dissection, we first create a window between the internal spermatic vessels and the external spermatic fascia so that the internal spermatic vessels are separate from the external spermatic fascia and its associated structures (cremasteric fibres, external spermatic vessels, vas deferens and its vessels).52 A second Penrose drain is then introduced between the internal spermatic vessels and the external spermatic fascia and its associated structures. We first dissect the contents of the internal spermatic fascia (lying on top of the most superficial Penrose drain). Subtle pulsations will usually reveal the location of the underlying internal spermatic artery (or arteries). Once identified, the artery is dissected free of all surrounding veins and encircled with a 2-0 silk ligature for identification. Care is taken to identify a number of lymphatics (usually 2–5 channels) and these are also encircled with a 2-0 silk ligature. All internal spermatic veins are clipped or ligated (with 4-0 silk) and divided. At the end of the first dissection, the cord is skeletonized so that only the identified artery (or arteries) and lymphatics are preserved. We then elevate and dissect the contents of the external spermatic fascia (lying between the 2 Penrose drains). The vas deferens and its associated vessels are readily identified and preserved. Any cremasteric artery is also preserved. The remaining cremasteric fibres and veins are ligated and cut thus skeletonizing the cord. At the completion of varicocelectomy, the cord should contain only the testicular artery or arteries, vas deferens, and associated vessels and spermatic cord lymphatics. The wound is irrigated with 1% Neomycin irrigation, and Scarpa's and Camper's fascia are closed with a single 3-0 chromic catgut suture. The incision is infiltrated with 0.5% Marcaine solution with epinephrine, and the skin is closed with a running 4-0 Vicryl subcuticular closure reinforced with Steri-Strips. A dry sterile dressing is applied. |

+91 - 95661 39630
+91 - 94441 68963



